VP4-2024: a Fight Against Cold Tumors
IBI363 is an experimental drug designed to tackle a significant challenge in cancer immunotherapy: the resistance of certain tumors to immune checkpoint inhibitors and their lack of immune cell infiltration, which leads to them being characterized as “cold” tumors. In cancer immunotherapy, “cold” tumors do not attract a substantial immune response. They have few infiltrating T cells and do not respond well to immunotherapies like checkpoint inhibitors. Checkpoint inhibitors, such as those targeting the programmed death-1 (PD-1) pathway, have transformed the treatment of various cancers by blocking inhibitory signals that prevent the immune system from attacking cancer cells. However, not all patients respond to these treatments, and resistance is a major issue. The dual mechanism of action of IBI363 described suggests that it is designed to overcome these challenges in two ways:
- Blocking PD-1 checkpoint: By inhibiting the interaction between PD-1 on T cells and its ligand PD-L1 on tumor cells, IBI363 could prevent the “off” signal that typically hampers T cell activity in the tumor microenvironment. This could release the brakes on the immune response, allowing T cells to attack cancer cells more effectively.
- Cis-activating α-biased IL-2: Interleukin-2 (IL-2) is a cytokine that plays a crucial role in the growth and activation of T cells. However, the use of IL-2 as a treatment has been limited by its toxicity and the fact that it can stimulate regulatory T cells (Tregs), which suppress immune responses. A cis-activating α-biased IL-2 is likely a modified form of IL-2 that preferentially stimulates effector T cells over Tregs, potentially enhancing the immune response against the tumor while minimizing side effects.
By revitalizing exhausted tumor-specific T cells, IBI363 could potentially convert “cold” tumors into “hot” tumors characterized by a strong immune cell presence and more responsiveness to immunotherapy. IBI363 would still be in the experimental stages, and its safety and efficacy would need to be established through clinical trials. The development of such therapies is part of ongoing research efforts to improve outcomes for patients with cancers that are currently difficult to treat with existing immunotherapies.
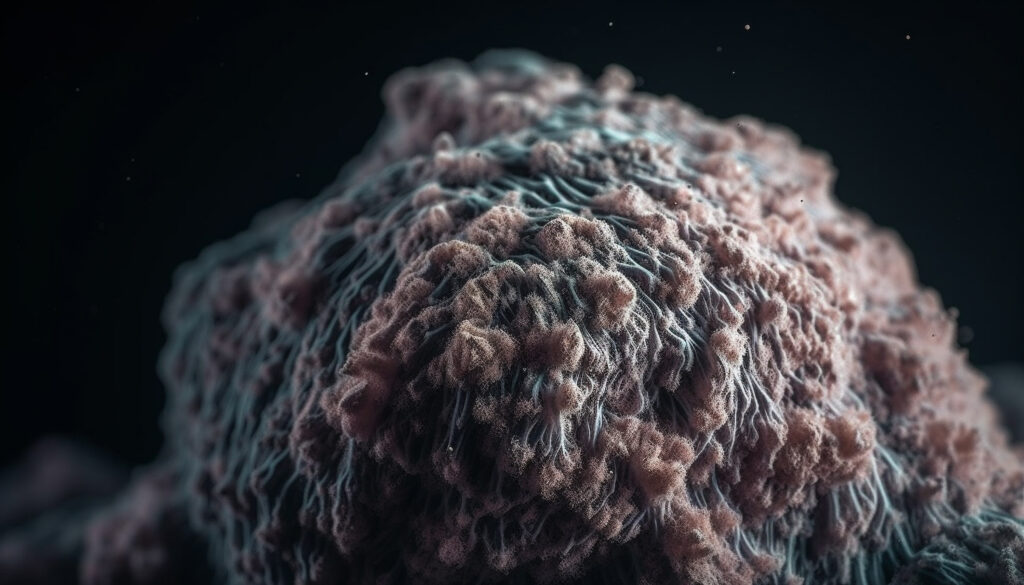
Pic: freepik, Source: <a href=”https://www.annalsofoncology.org/article/S0923-7534(24)00679-3/fulltext?rss=yes”>Link</a>