Transition to Personalized Oncology in Liver Cancer
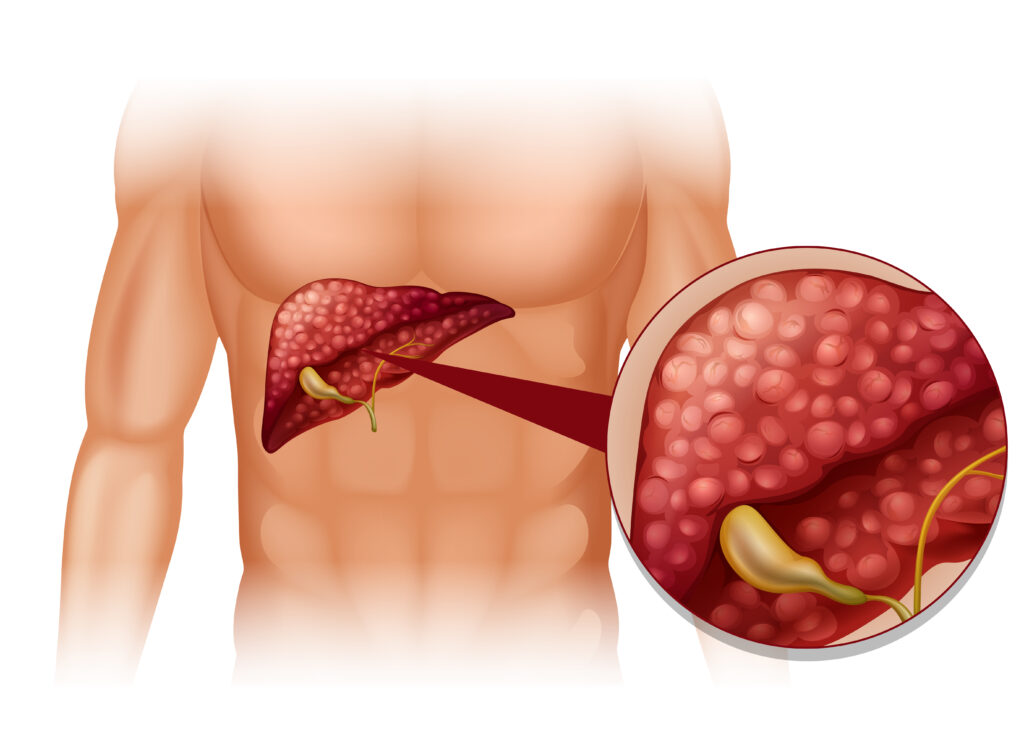
Radioembolization is a form of radiation therapy used to treat liver tumors. Radioactive microspheres are injected into the arteries that feed the tumor. The goal is to deliver a high radiation dose directly to the cancer cells while sparing the surrounding healthy tissue.
Technetium-99m macroaggregated albumin (99mTc-MAA) is a radiopharmaceutical used in nuclear medicine for various diagnostic purposes, including the simulation of radioembolization. When used in this context, 99mTc-MAA is injected into the hepatic artery, and its distribution within the liver is imaged using SPECT combined with CT (SPECT/CT). This imaging helps to predict the distribution of the actual therapeutic microspheres and to calculate the radiation dose that the tumor and the non-tumor liver tissue will receive during the actual treatment.
The study’s aim to establish novel dose limits for 99mTc-MAA SPECT/CT is crucial because it would help to:
- Optimize Treatment: By accurately predicting the radiation dose distribution, physicians can tailor the treatment to each patient’s specific anatomy and tumor characteristics, potentially improving outcomes.
- Enhance Safety: Establishing safe dose limits is essential to minimize the risk of radiation-induced liver disease (RILD) and other complications associated with radioembolization.
- Facilitate Clinical Transition: The study could help overcome the barriers to its clinical adoption by demonstrating the safety and efficacy of 99mTc-MAA SPECT/CT in pretreatment planning.
To achieve these goals, the study would likely involve a combination of retrospective analysis of patient data, prospective clinical trials, and advanced dosimetric calculations. The researchers would need to correlate the SPECT/CT imaging data with patient outcomes, including tumor response and the incidence of adverse effects, to determine the optimal and safe dose limits for pretreatment planning.
The key findings regarding the transition from non-personalized to personalized treatment planning in liver cancer patients undergoing radioembolization included the significant undertreatment of patients when comparing the BSA method with planar-based treatment planning, with reductions in calculated activities of up to 61.9% . Additionally, personalized dosimetry improved patient outcomes compared to standard manufacturing guidelines.
The study validated the effectiveness of the newly established SPECT/CT dose limits by comparing the resulting activity calculations with those determined by planar imaging and evaluating three different treatment plans using the established safety constraints. The dose limits were found to be safe for 97.5% of treated patients, demonstrating the successful application of these limits in the majority of cases.
The findings from such a study could have significant implications for interventional oncology, potentially leading to more personalized and effective treatments for patients with liver tumors. Potential challenges or barriers to the clinical adoption of 99mTc-MAA SPECT/CT in pretreatment planning include the unknown safety constraints for SPECT/CT and differences in dose limits between planar imaging and SPECT/CT. However, the clinical implementation of the findings would require careful consideration of the cost-effectiveness, training requirements for clinicians, and the integration of the new protocols into existing treatment workflows.
Pic by freepik, Source: <a href=”https://www.redjournal.org/article/S0360-3016(24)00008-7/fulltext?rss=yes%22%3ELink%3C/a>